Archive for the ‘ALS Research – Other’ Category
2
Mar
Posted by alsresearchnews in ALS Research - Other. Tagged: ALS, C9ORF72, Lou Gehrig's Disease, Resarch. Leave a comment
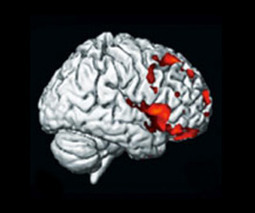
Via Scoop.it – ALS Lou Gehrig’s Disease
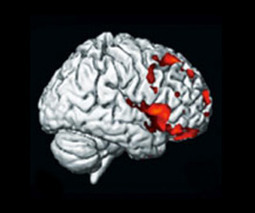 Neurologists may need to keep an eye out for cognitive and behavioral changes in people showing signs of ALS, according to a new study. The research team, led by Trinity College Dublin neurologist Orla Hardiman MD FRCP, found that 50% of people examined with the most common form of familial ALS identified to date also showed signs of frontotemporal lobar degeneration (FTLD). The brain disorder might result in difficulties in critical thinking, problem solving and making complex decisions. The study, which included 20 people with familial ALS harboring repeat expansions in the C9ORF72 gene, is the first to clinically describe this form of ALS. The study is one of three studies this month that confirms that repeat expansions in the C9ORF72 gene are the most common cause of inherited forms of ALS, ALS-FTLD and FTLD.
Neurologists may need to keep an eye out for cognitive and behavioral changes in people showing signs of ALS, according to a new study. The research team, led by Trinity College Dublin neurologist Orla Hardiman MD FRCP, found that 50% of people examined with the most common form of familial ALS identified to date also showed signs of frontotemporal lobar degeneration (FTLD). The brain disorder might result in difficulties in critical thinking, problem solving and making complex decisions. The study, which included 20 people with familial ALS harboring repeat expansions in the C9ORF72 gene, is the first to clinically describe this form of ALS. The study is one of three studies this month that confirms that repeat expansions in the C9ORF72 gene are the most common cause of inherited forms of ALS, ALS-FTLD and FTLD.
Via blogs.als.net
2
Mar
Posted by alsresearchnews in ALS Research - Other. Tagged: ALS, BMAA, Lou Gehrig's Disease, Resarch. Leave a comment
Via Scoop.it – ALS Lou Gehrig’s Disease

A prominent botanist with a passion for preserving the rainforest and exploring medicines in native cultures is helping to make inroads into one of the most difficult problems in medical research: understanding and treating the neurological diseases Alzheimers, Parkinsons and amyotrophic lateral sclerosis, or ALS, better known as Lou Gehrig’s disease. The botanist is Paul Allan Cox, whose studies of plants and human diets on Guam a decade ago have led to one of the most promising approaches to understanding the diseases, which afflict millions worldwide. In 2003, Cox showed that a natural neurotoxin called BMAA becomes concentrated in the diets of certain Guananian villagers, who then develop some of the world’s highest rates of ALS. Since then, he and researchers around the world have found elevated levels of BMAA in the brains of Alzheimer’s and ALS patients in North America. They have identified a universal source of BMAA in blue-green algae called cyanobacteria that are found nearly everywhere. Now, they have taken early steps to explore the detailed biophysical role that BMAA may be playing in causing the failure of human motor neurons. Ever one to explore native cultures, Cox has even found an unusually healthy village on the Japanese island of Okinawa where exceptionally long-lived residents might offer clues to something neurologically protective in the diet. Cox discussed his findings at Livermore’s Bankhead Theater last week as part of the Rae Dorough Speaker’s Series.
Via www.independentnews.com
29
Feb
Posted by alsresearchnews in ALS Research - Other. Tagged: ALS, Lou Gehrig's Disease, Resarch. Leave a comment
Via Scoop.it – ALS Lou Gehrig’s Disease
 In science, refuting a hypothesis can be as significant as proving one, all the more so in research aimed at elucidating how diseases proceed with a view toward preventing, treating, or curing them. Such a discovery can save scientists from spending precious years of effort exploring a dead end. In a study published in the Proceedings of the National Academy of Sciences, Munich-based researchers refute a widely accepted hypothesis about a causative step in neurodegenerative conditions. These results deal specifically with animal models of human amyotrophic lateral sclerosis (ALS, aka Lou Gehrig’s disease) but also raise questions for research on other neurodegenerative diseases, such as Alzheimer’s or Huntington’s disease.
In science, refuting a hypothesis can be as significant as proving one, all the more so in research aimed at elucidating how diseases proceed with a view toward preventing, treating, or curing them. Such a discovery can save scientists from spending precious years of effort exploring a dead end. In a study published in the Proceedings of the National Academy of Sciences, Munich-based researchers refute a widely accepted hypothesis about a causative step in neurodegenerative conditions. These results deal specifically with animal models of human amyotrophic lateral sclerosis (ALS, aka Lou Gehrig’s disease) but also raise questions for research on other neurodegenerative diseases, such as Alzheimer’s or Huntington’s disease.
Via www.eurekalert.org
29
Feb
Posted by alsresearchnews in ALS Research - Other. Tagged: ALS, Lou Gehrig's Disease, Resarch, zebrafish. Leave a comment
Via Scoop.it – ALS Lou Gehrig’s Disease
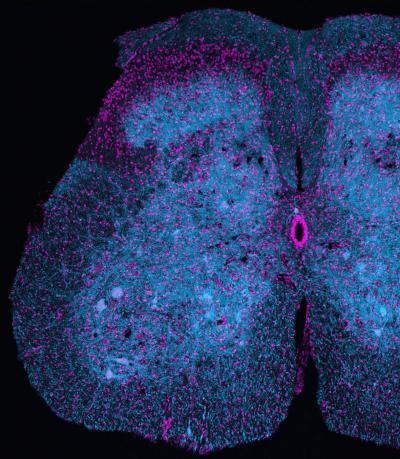
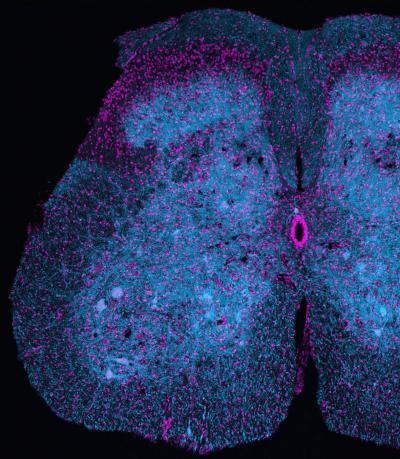
 The quest for treatments for motor neurone disease, spinal cord injury and strokes could be helped by new research that shows how key cells are produced. Scientists at the University of Edinburgh have been able to manipulate the production of motor neurones – which control all muscle activity – in zebrafish. Zebrafish are important in helping scientists understand how motor neurones are produced, because unlike mammals, they are able to create new motor neurones as adults. Humans can generate motor neurones during embryonic development but lose the ability to generate these cells, which are important for speaking, walking and breathing, after birth. This means that the body is unable to replace these cells if they become damaged as a result of motor neurone disease, stroke or spinal cord injury.
The quest for treatments for motor neurone disease, spinal cord injury and strokes could be helped by new research that shows how key cells are produced. Scientists at the University of Edinburgh have been able to manipulate the production of motor neurones – which control all muscle activity – in zebrafish. Zebrafish are important in helping scientists understand how motor neurones are produced, because unlike mammals, they are able to create new motor neurones as adults. Humans can generate motor neurones during embryonic development but lose the ability to generate these cells, which are important for speaking, walking and breathing, after birth. This means that the body is unable to replace these cells if they become damaged as a result of motor neurone disease, stroke or spinal cord injury.
Via www.eurekalert.org
29
Feb
Posted by alsresearchnews in ALS Research - Other. Tagged: ALS, Lou Gehrig's Disease, Resarch. Leave a comment
Via Scoop.it – ALS Lou Gehrig’s Disease
Animals regulate body weight using an exquisitely tuned system. If the body needs fuel, the animal can go in search of food. Any extra fuel is stored as fat, to be used when energy stores run low. Through a complex series of checks and balances, animals (including humans) generally maintain a stable body weight, where energy consumed equals energy used. In ALS patients, however, something throws off this balance. Besides the symptoms stemming from deteriorating motor neurons, such as difficulties walking, talking, breathing, and even swallowing, ALS patients often lose weight. Although some of this weight loss is perhaps due to muscle wasting, scientists have also noticed that ALS patients often lose a significant amount of body fat. When Robert Kalb, a neuroscientist at the Children’s Hospital of Philadelphia, and his colleagues searched the research literature, however, they realized that no one really knew what caused weight to drop in ALS. Nor did scientists know whether the weight loss contributed to the progression of ALS. A series of experiments in tissue culture and in the model organism Caenorhabditis elegans showed that ALS patients have a metabolic abnormality that contributes to both weight loss and the progression of disease.
Via www.alscenter.org
29
Feb
Posted by alsresearchnews in ALS Research - Other. Tagged: ALS, Lou Gehrig's Disease, New York, Resarch. Leave a comment
Via Scoop.it – ALS Lou Gehrig’s Disease

On February 9 and 10, ALS researchers from P2ALS and several different pharmaceutical companies gathered in New York as part of the semi-annual meetings of P2ALS. P2ALS was founded in 2010 as a joint effort between The Robert Packard Center for ALS Research and Project A.L.S. with the goal of finding new treatments for ALS. This collaboration established a highly cooperative network of scientists that share unpublished findings to facilitate rapid testing and verification of complex research questions posed by ALS. Initially, P2ALS focused on genetics, and motor neuron and glial biology– basic science that allowed the identification of pathogenic pathways in ALS and potential therapeutic targets. At this most recent meeting held in New York City, the headquarters of Project A.L.S., scientists from around the world shared their most recent research, which covered advances in motor neuron and astrocyte biology, the genetics of familial and sporadic ALS, including new avenues of study opened up by the discovery of the C9ORF72 gene, and recent progress in the use of stem cells in the study and treatment of ALS.
Via www.alscenter.org
27
Feb
Posted by alsresearchnews in ALS Research - Other. Tagged: ALS, Lou Gehrig's Disease, Resarch. Leave a comment
Via Scoop.it – ALS Lou Gehrig’s Disease
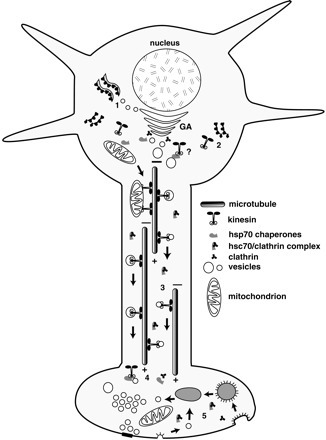
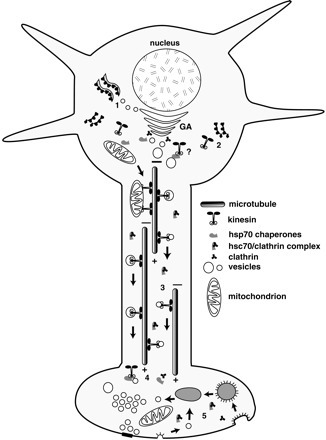 Mitochondria produce the energy needed to keep muscles healthy and moving. But in people with ALS, these power plants go out of service likely contributing to muscle atrophy and ultimately, paralysis. Scientists are developing treatments to supe up mitochondria in hopes to keep the energy flowing in the muscles and connecting nerves. One of these emerging medicines, Knopp Biosciences’ dexpramipexole now licensed by Biogen Idec, is gathering steam as a potential ALS treatment strategy. Reporting phase II results last fall, neurologists found that the drug slowed disease progression about 30%. Some researchers suspect however, that these mitochondrial-targeted medicines may need to do much more than boost energy production to grind ALS to a halt. Even operating at full steam, these power plants may be unable to provide enough energy to keep muscles working because they may not be in the right place to do their job. Scientists are now beginning to understand why these mitochondria might stray, suggesting new strategies to tackle the disease.
Mitochondria produce the energy needed to keep muscles healthy and moving. But in people with ALS, these power plants go out of service likely contributing to muscle atrophy and ultimately, paralysis. Scientists are developing treatments to supe up mitochondria in hopes to keep the energy flowing in the muscles and connecting nerves. One of these emerging medicines, Knopp Biosciences’ dexpramipexole now licensed by Biogen Idec, is gathering steam as a potential ALS treatment strategy. Reporting phase II results last fall, neurologists found that the drug slowed disease progression about 30%. Some researchers suspect however, that these mitochondrial-targeted medicines may need to do much more than boost energy production to grind ALS to a halt. Even operating at full steam, these power plants may be unable to provide enough energy to keep muscles working because they may not be in the right place to do their job. Scientists are now beginning to understand why these mitochondria might stray, suggesting new strategies to tackle the disease.
Via blogs.als.net
26
Feb
Posted by alsresearchnews in ALS Research - Other. Tagged: ALS, Lou Gehrig's Disease, Resarch. Leave a comment
Via Scoop.it – ALS Lou Gehrig’s Disease
 Several neurodegenerative diseases – including Alzheimer’s and ALS (Lou Gehrig’s disease) – are caused when the body’s own proteins fold incorrectly, recruit and convert healthy proteins to the misfolded form, and aggregate in large clumps that gum up the works of the nervous system. “For Star Trek fans, this is like the Borg, [a fictional race of cyborgs that abduct and assimilate humans and other species],” says Steven Plotkin, a biophysicist at the University of British Columbia in Vancouver who studies the process of protein misfolding. Plotkin’s team has developed an algorithm that can predict which regions of a protein are prone to exposure upon misfolding, and how mutations in the protein and changes in the cellular environment might affect the stability of these vulnerable regions. These predictions help scientists gain a better understanding of protein dynamics, and may one day help in developing treatments to effectively combat currently incurable neurodegenerative diseases. The team will present its findings at the 56th Annual Meeting of the Biophysical Society (BPS), held Feb. 25-29 in San Diego, Calif.
Several neurodegenerative diseases – including Alzheimer’s and ALS (Lou Gehrig’s disease) – are caused when the body’s own proteins fold incorrectly, recruit and convert healthy proteins to the misfolded form, and aggregate in large clumps that gum up the works of the nervous system. “For Star Trek fans, this is like the Borg, [a fictional race of cyborgs that abduct and assimilate humans and other species],” says Steven Plotkin, a biophysicist at the University of British Columbia in Vancouver who studies the process of protein misfolding. Plotkin’s team has developed an algorithm that can predict which regions of a protein are prone to exposure upon misfolding, and how mutations in the protein and changes in the cellular environment might affect the stability of these vulnerable regions. These predictions help scientists gain a better understanding of protein dynamics, and may one day help in developing treatments to effectively combat currently incurable neurodegenerative diseases. The team will present its findings at the 56th Annual Meeting of the Biophysical Society (BPS), held Feb. 25-29 in San Diego, Calif.
Via www.medicalnewstoday.com
23
Feb
Posted by alsresearchnews in ALS Research - Other. Tagged: ALS, BMAA, Lou Gehrig's Disease, Resarch. Leave a comment
Via Scoop.it – ALS Lou Gehrig’s Disease
 As a top marine researcher, Dr. Neil Hammerschlag, scours the oceans in search of sharks.On a recent afternoon aboard a research boat, Hammerschlag and his team from the University of Miami’s Rosenstiel School of Marine and Atmospheric Science, found what they refer to as an “amazing” creature. Hammerschlag studies the mythical sea creatures to discover how their ailments could be linked to the development of human diseases. What they found in the shark fin? The neurotoxin BMAA (short for B-Methylamino-L-alanine), which is produced by an algae known as cyanobacteria, often found in lakes, oceans and the soil. This toxin has been shown to damage neurons. Neurons are the primary building block of the brain.” The toxin, which has been shown to kill brain cells, has turned up – repeatedly – in Mash’s studies of the human brain — particularly of the brains of victims of Alzheimer’s, Parkinson and Lou Gehrig’s patients. “We are detecting BMAA in the brains of the patients that have donated them for research,” Mash said. “That is why we are seeing linkage with Alzheimer’s and with Lou Gehrig’s disease.” If the shark holds clues to brain-based diseases that have the potential to affect everybody — it’s even more chilling that the shark is threatened today because of a demand for soup made from its fin.
As a top marine researcher, Dr. Neil Hammerschlag, scours the oceans in search of sharks.On a recent afternoon aboard a research boat, Hammerschlag and his team from the University of Miami’s Rosenstiel School of Marine and Atmospheric Science, found what they refer to as an “amazing” creature. Hammerschlag studies the mythical sea creatures to discover how their ailments could be linked to the development of human diseases. What they found in the shark fin? The neurotoxin BMAA (short for B-Methylamino-L-alanine), which is produced by an algae known as cyanobacteria, often found in lakes, oceans and the soil. This toxin has been shown to damage neurons. Neurons are the primary building block of the brain.” The toxin, which has been shown to kill brain cells, has turned up – repeatedly – in Mash’s studies of the human brain — particularly of the brains of victims of Alzheimer’s, Parkinson and Lou Gehrig’s patients. “We are detecting BMAA in the brains of the patients that have donated them for research,” Mash said. “That is why we are seeing linkage with Alzheimer’s and with Lou Gehrig’s disease.” If the shark holds clues to brain-based diseases that have the potential to affect everybody — it’s even more chilling that the shark is threatened today because of a demand for soup made from its fin.
Via miami.cbslocal.com
22
Feb
Posted by alsresearchnews in ALS Research - Other. Tagged: ALS, Lou Gehrig's Disease, Resarch. Leave a comment
Via Scoop.it – ALS Lou Gehrig’s Disease

The American Academy of Neurology and the ALS Association are awarding the 2012 Sheila Essey Award: An Award for ALS Research to Christopher Shaw, MBChB, MD, FRACP, with the Institute of Psychiatry at King’s College London. Shaw will receive the award during the Academy’s 64th Annual Meeting, April 21-28, 2012, in New Orleans. The Annual Meeting is the world’s largest gathering of neurologists with more than 10,000 attendees and more than 2,300 scientific presentations on the latest research advance in brain disease. Shaw is receiving the award for his research investigating mutated genes for answers as to how and why some people get ALS. Many mutated genes increase disease risk by causing toxic proteins to form clumps in the brain, which causes neurodegeneration. Shaw’s research has focused on a specific toxic protein called TDP-43, which is found in about 95 percent of all people with ALS.
Via www.aan.com